Phlebeurysmis a pathological condition characterized by a change in the structure of the venous system, leading to an increase in the diameter of the lumen of the superficial veins and disruption of the valve system, manifested in valve failure, i. e. in their incomplete closure of the vein.
Normally, blood flows through the veins against the force of gravity - from bottom to top, which is possible solely due to the work of the venous valves. Under the influence of a number of reasons, primary (due to changes in the valve itself) or secondary (due to dilation of the vein) valve failure occurs; this condition is characterized by incomplete closure of the venous valve and reverse blood flow. The reverse flow of blood aggravates changes in the venous wall, and also contributes to stagnation of blood in the lower extremities, causing swelling of the lower extremities and a feeling of heaviness in the legs.
In addition to stagnation of blood in the lower extremities, the above processes lead to disruption of the linear flow of blood through the veins from top to bottom, the appearance of reflux (reverse blood flow) and turbulent blood flows in the area of expansion. Changes in blood flow characteristics are the leading cause of thrombosis.
Possible causes of the development of varicose veins of the lower extremities
- Physical inactivity- the leading cause of varicose veins. A sedentary lifestyle and prolonged sitting position contribute to prolonged high load on the vein valves. During physical activity - walking, running, swimming - constantly working muscles on the thigh and lower leg help to "expel" blood from the venous system of the lower extremities. Static sitting in a sitting position for a long time leads to increased load on the venous valves and, over time, the venous valves, unable to withstand the load, may cease to perform their function in full.
- Obesityshould be considered the second most important reason. Heavy weight also increases the load on the valve system of the veins of the lower extremities, contributing to the disruption of their proper functioning.
- Pregnancyis the third most common cause. Hormonal changes, increased body weight, compression of the pelvic veins by the fetus are sufficient reasons for dysfunction of the venous valves. However, up to 50% of changes in the venous wall detected during pregnancy are functional in nature and disappear on their own within the first year after birth.
- Smoking– the fourth most common cause of varicose veins. Changes in the venous wall can be associated with the unfavorable effect of the composition of smoking mixtures on the tone of the venous wall.
- Heredity– another possible reason for the development of varicose veins. It is generally accepted that heredity plays a leading role in the development of varicose veins, however, genes responsible for the development of varicose veins have not yet been discovered; it is generally accepted that genes responsible for changes in the structure of connective tissue structures are the leading cause of varicose veins. However, the influence of heredity can be greatly exaggerated, and lifestyle changes, normalization of body weight and smoking cessation will help to avoid varicose veins even in patients with an unfavorable hereditary history.
Signs of varicose veins
- Presence of dilated saphenous veins, the non-linear course of the vein is the most objective, but not the only manifestation of varicose veins. Often, even veins dilated several times may not be visible, especially with a pronounced subcutaneous layer.
- Edema of the lower extremitiesat the end of the working day, especially with asymmetrical swelling, are the earliest and most common sign of varicose veins.
- You should also think about the presence of varicose veins whenpresence of heaviness in the legsin the evening and at night, leg cramps at night.
- Spider veins and venous patternintradermal veins, although they are more of an aesthetic problem, may also indicate the presence of changes in the saphenous veins.
- Persistent redness, skin thickening, lipodermatosclerosis, trophic ulcers on the foot and leg indicate a decompensated course of varicose veins.
Diagnosis of varicose veins
The diagnosis of varicose veins of the lower extremities can be made only on the basis of ultrasound diagnostic data.
During ultrasound scanning of the veins of the lower extremities, the doctor examines in detail the features of the deep and superficial veins from the groin to the ankle, measuring the diameter of the veins, analyzing the features of blood flow in the veins, and detects the presence of reflux. Based on the data obtained, the doctor forms a conclusion.
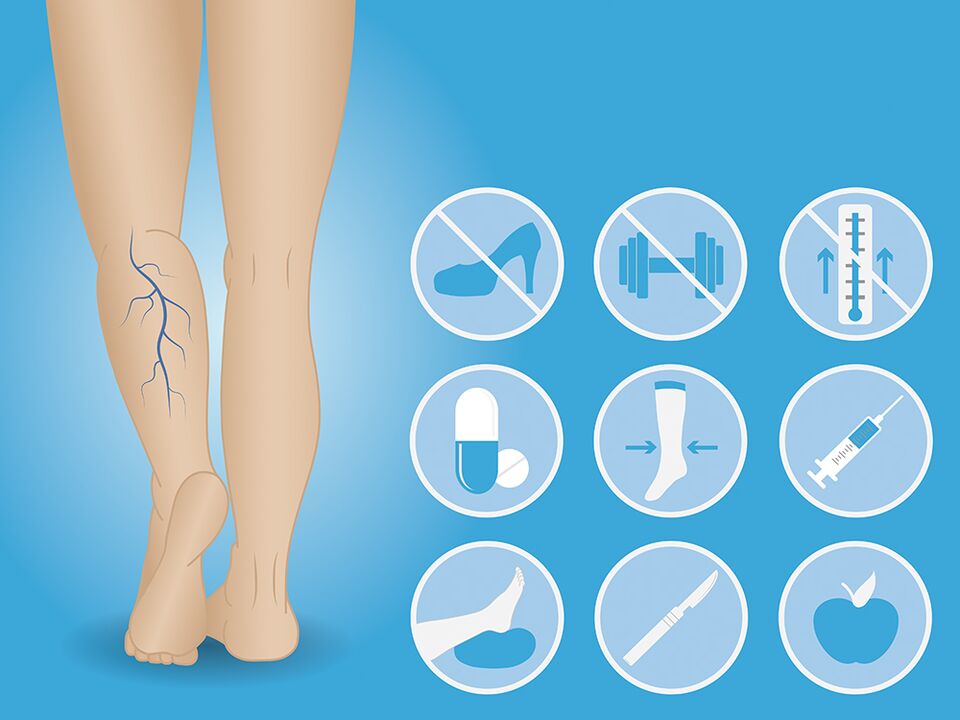
Prevention of varicose veins
Prevention of varicose veins is a rational motor regimen, normalization of body weight, and quitting smoking.
If there are initial signs of varicose veins, venotonics and wearing compression stockings will help reduce the rate of progression of the disease.
Compression hosiery should be selected by a doctor depending on the severity of varicose veins and the patient’s anthropometric data.
Treatment of varicose veins
Treatment of varicose veins is exclusively surgical.
At the moment, many different methods of surgical treatment have been developed - from open techniques - combined phlebectomy to minimally invasive methods - laser or radiofrequency coagulation of veins, mechanochemical methods.
- Varicose veins can be removed using a miniphlebectomy, a technique in which the varicose veins are removed from the subcutaneous tissue from separate punctures and bandaged.
- Small varicose veins can be removed using sclerotherapy - the introduction of a special glue-like substance - sclerosant - into the venous lumens.
- Spider veins and intradermal veins can be removed using sclerotherapy.
However, even after fully completed treatment, the risk of recurrence of varicose veins of the lower extremities is 10-15%. Adequate physical activity, playing sports (running, walking, exercise bike, swimming), normalizing body weight and giving up bad habits will help reduce the likelihood of relapse after surgical treatment. Periodic use of phlebotonics and wearing properly selected compression stockings will help reduce the rate of spread.
The main thing is not to delay seeing a doctor!

















